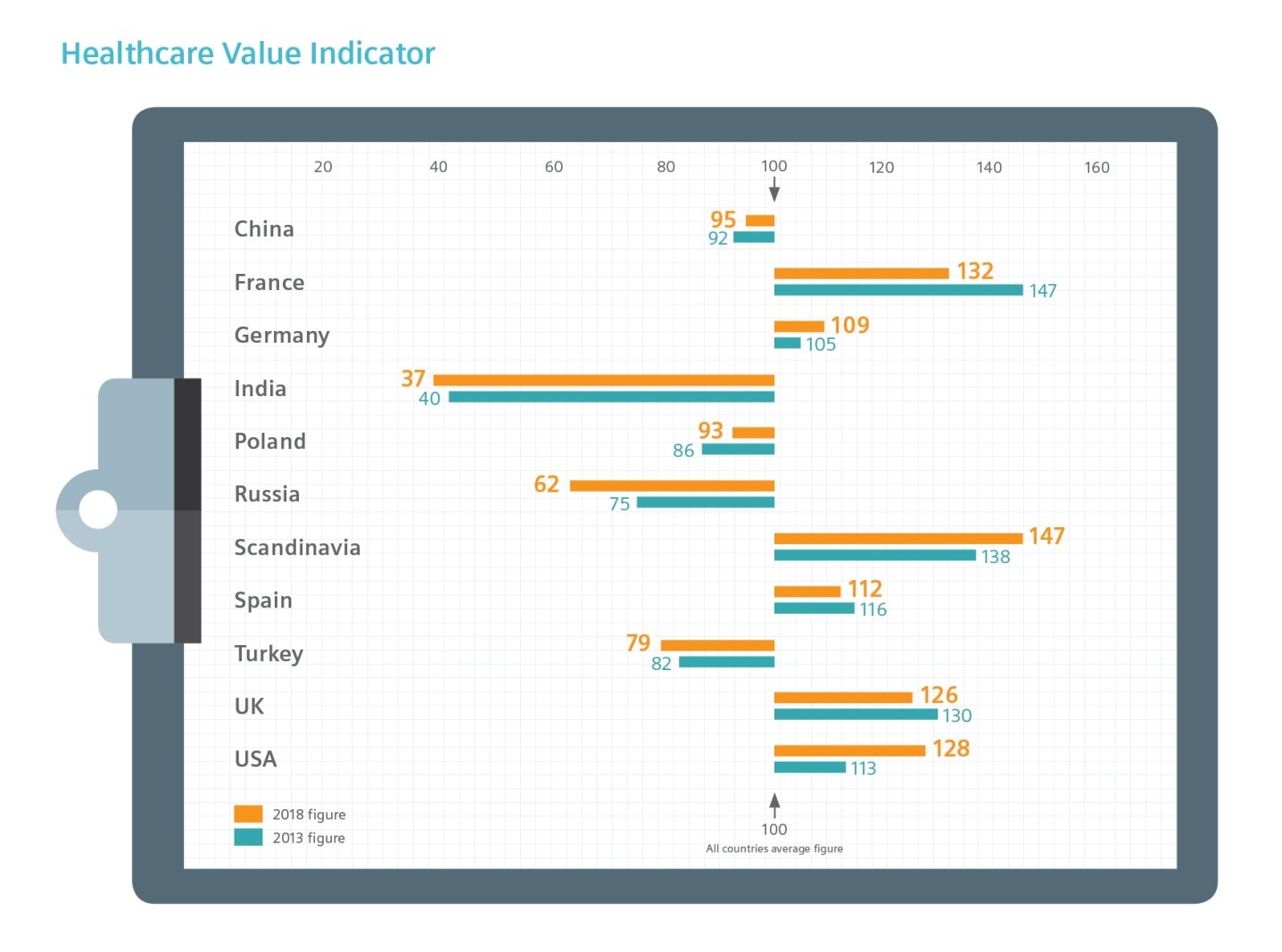
- New global research from Siemens Financial Services relates healthcare demand and resources to the patient outcomes they produce, resulting in a ‘healthcare value indicator’
- This model was built in consultation with healthcare experts/practitioners around the world and uses a wide range of official data sources
- Pressures relating to application of funds, infrastructure and skills and considered against patient outcomes such as immunisation levels, life expectancy and quality of life indicators
- Access to the latest technology and equipment can help improve a country’s healthcare value indicator, but pressure on budgets makes investment difficult
- The study estimates the amount of private finance available across the globe that can unlock ‘frozen’ capital, otherwise tied up in capital equipment and technology purchases
- Finance can help ease the pressure on healthcare organisations as they struggle to find ways to transform care delivery and embrace digitalisation
Siemens Financial Services (SFS) has released a new research paper which examines the pressures on resources for healthcare systems around the world, the patient outcomes they are delivering, and the ‘value’ each healthcare system is producing. Access to advanced medical technology is a key factor that enables better patient outcomes and improved healthcare value.
The paper therefore examines the role that private finance can play in enabling better access to advanced equipment and technology, along with an estimate of the capital currently ‘frozen’ in equipment purchase that could be freed for immediate and urgent operational priorities and healthcare transformation initiatives.
Healthcare systems around the world are under pressure. Mature healthcare systems, such as in Europe and the USA, are feeling the pressure of reform. Developing healthcare systems, such as Turkey, Russia, China and India are battling to keep up with the pressure of accelerating expectations and demand.
The extent of pressure exerted on healthcare resources can be broadly determined by three categories: application of funds, infrastructure and skills. Patient outcomes were assessed in terms of morbidity rates, survival rates and official quality of life measures. SFS’ research model then expresses patient outcomes as a simple ratio of resource pressure to give an idea of the ‘value’ the health system is delivering. For example, if a health system is well-resourced (low pressure) and producing better outcomes (high score) then the Value Indicator will be higher.
Up-to-date technology is one critical element that relieves pressure on healthcare systems by optimising clinical and care skills. Budgets remain under pressure in all healthcare systems, however, the balance of required technology upgrade and investment burden is a consistent factor across all the countries featured in the study.
SFS’ research estimates the volumes of finance that could be ‘unlocked’ from key equipment and technology capital investment and applied to urgent operating finance requirements. This is achieved by deploying private sector finance techniques that align payments with the benefits of upgraded medical technology.
| Frozen capital | 2017 Estimate ($ billion) |
| China | 16.53 |
| India | 1.3 |
| France | 3.68 |
| Germany | 6.47 |
| Poland | 0.61 |
| Russia | 1.2 |
| Scandinavia | 1.56 |
| Spain | 1.39 |
| Turkey | 0.77 |
| UK | 1.89 |
| USA | 34.78 |
“There are a number of specialist financing methods that are being deployed by healthcare institutions to upgrade their medical technology, and support the transformation of healthcare delivery,” says Chris Wilkinson, Head of Sales for Healthcare and Public Sector for Siemens Financial Services in the UK. “These methods, such as ‘pay to access/use’, asset-based lending and others, cover the range of requirements, from the acquisition of a single piece of equipment, to financing a whole new healthcare facility. Healthcare organisations then free up precious capital, which can be used to improve the value derived from the healthcare system by relieving pressure on resources and maximising patient outcomes.”
[1] Sources include: World Health Organization; OECD; National Departments of Health; The Lancet; Chinese Statistical Yearbook; World Bank; International Diabetes Federation; Emergo; National Trade (Export) Departments; Global Cancer Observatory; Global Health Observatory; COCIR; Wiley Inc; Medical peer-review journals (various)